Prostate cancer is the most commonly diagnosed cancer in men in the UK, with about 1 in 8 men diagnosed in their lifetime, leading to more than 12,000 deaths each year.
Despite an increase in available therapies, prostate cancer incidence rates are projected to increase by 15% in the UK over the next five years.
We must continue to raise awareness of this devastating disease beyond awareness days and months by shining a light on the risk factors, the early signs and symptoms, and the need for increased testing.
Early diagnosis is vital in cancer of the prostate, with the five-year survival rate for most patients with local (disease at an early stage) prostate cancer being nearly 100%. Compare this to patients with advanced prostate cancer, and the five-year survival rate falls to 49%.
What is prostate cancer?
Prostate cancer is when the cells in the prostate gland grow uncontrollably and abnormally until a tumour develops. Many prostate cancers grow slowly and are confined to the prostate gland, where they may not cause serious harm.
However, while some types of prostate cancer grow slowly and may need minimal or even no treatment, other types are aggressive and can spread quickly. Prostate cancer that’s detected early, when it’s still confined to the prostate gland, has the best chance for successful treatment.
Overcoming a silent disease
Prostate cancer is notorious for the fact that it shows very few symptoms in the early curable stages of the disease, leading to nearly half of all cases being diagnosed at an advanced or metastatic stage, (see table below for an explanation of the stages). ,
Those with early prostate cancer won’t experience any signs or symptoms of the disease, further highlighting the importance for men to know and understand the risk factors.
By striving for early diagnosis, we have an opportunity to reduce the risk of developing advanced disease. This will then help patients to maintain a good quality of life and reduce the risk of death.
Determining the stage (extent) of prostate cancer plays a key role in deciding on treatment options. But imaging tests for prostate cancer such as CT and MRI scans can’t detect all areas of cancer, especially small areas of cancer in lymph nodes, so doctors are now looking at newer types of imaging tests.
Risk factors – are you at risk?
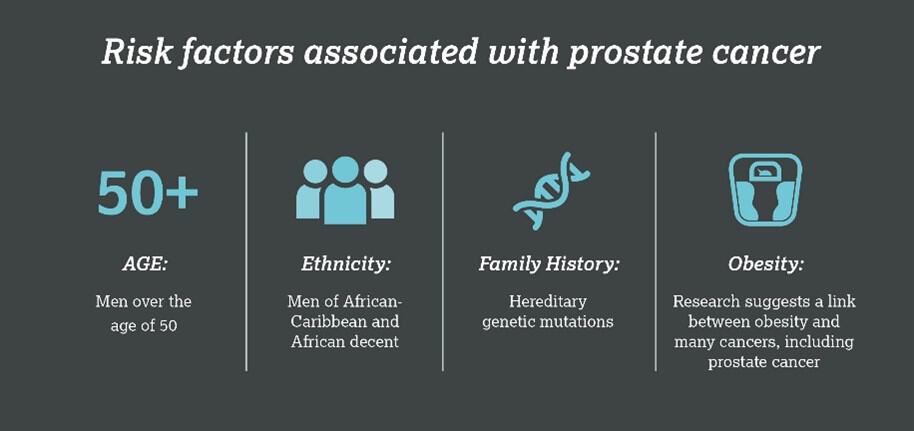
The cause of prostate cancer is unknown but there are factors that can increase your risk. Having one or more risk factors does not mean you will get prostate cancer. Risk factors for prostate cancer include:
• Older age. Your risk of prostate cancer increases as you age. Most cases are diagnosed in men over 50 years of age (most commonly ages 75 to 79). If you’re under 50, your risk of being diagnosed with prostate cancer is very low, but it is still possible.
• Ethnicity. For reasons not yet determined, Black people have a greater risk of prostate cancer than people of other races.11 In Black people, prostate cancer is also more likely to be aggressive or advanced.
• Family history. If a blood relative has been diagnosed with prostate cancer, your risk may be increased. 10% to 20% of all prostate cancer cases are hereditary and are usually due to a single inherited genetic mutation, such as BRCA1 or BRCA2. A BRCA mutation may also increase a man’s risk of being diagnosed with a more aggressive form of prostate cancer.
• Obesity. Recent research suggests there may be a link between obesity and prostate cancer, and that a balanced diet and regular exercise can lower your risk of developing prostate cancer. Being obese may also increase the risk of having a faster-growing type of prostate cancer.
Men with any of the above risk factors are advised to speak to their GP to discuss their concerns and any recommendations the GP may have.
Approaches to diagnosing prostate cancer
The PSA test – is a blood test that measures the amount of prostate-specific antigen (PSA) in your blood. PSA is a protein produced by normal cells in the prostate and by prostate cancer cells.
It’s normal to have a small amount of PSA in your blood, and the amount rises slightly as you get older, and your prostate gets bigger. A raised PSA level may suggest you have a problem with your prostate, but not necessarily cancer.
The digital rectal examination – a physical examination used routinely and extensively in primary care for prostate cancer.
Genomic testing – by looking at the genetic makeup of the prostate cancer, genomic tests may help predict whether a person’s prostate cancer will spread. Not all prostate cancers are the same.
Genomic profiling or molecular testing can assess the presence of inherited or non-hereditary gene mutations.
A germline (hereditary) mutation can be identified using a blood or saliva test to compare the sample against the known genome. Somatic (non-hereditary) mutations are acquired during natural cell division or from exposure to environmental factors throughout someone’s life.
As these non-hereditary mutations will only be present in cells arising from the original mutated cell, they are usually only tested once a tumour has formed, by taking a tissue sample from the tumour and testing for gene alterations.
Specialist MRI scan – latest national guidance recommends that all men suspected of having prostate cancer that has not spread outside the prostate gland should be offered a specialist MRI scan – multiparametric MRI (mpMRI).
The benefit of having mpMRI is that fewer men may need to go on to have a prostate biopsy, which has its own risks.
Prostate biopsy – A biopsy of the prostate gland is a medical procedure that involves taking a small sample of prostate tissue so it can be examined under a microscope to help diagnose prostate cancer.
If prostate cancer has already been diagnosed, a biopsy can also be used to assess the cancer grade, which predicts how fast the cancer will grow and how likely it is to spread, and it can help to guide the most effective, individual treatment option.
As with any medical procedure, there are side effects associated with a biopsy including pain or discomfort, short-term bleeding, infection and acute urine retention, whereby a small number of men find they suddenly can’t urinate after a biopsy which can be painful.
To screen or not to screen with the PSA test – a hot topic in the UK
There is currently no screening programme for prostate cancer in the UK – a topic which has been heavily debated within the medical community across the country.
While we know testing more men can reduce the number of cancer deaths due to early detection, concerns remain that the benefits do not outweigh the risks associated with screening.26
The Prostate-Specific Antigen (PSA) test is the most common initial test carried out for men.26
While evidence has shown using the PSA test to identify prostate cancer can save lives, the test can also produce unreliable results and can suggest prostate cancer when no cancer exists (a false-positive result), often leading to unnecessary biopsies.
Conversely, according to the NHS, around 1 in 7 of those with normal PSA levels may have prostate cancer (a false-negative result), so many cases may be missed.
For these reasons, the UK NHS Prostate Cancer Risk Management Programme’s (PCRMP) current guidelines do not support the PSA test as the basis for a screening programme.
This recommendation is likely to be challenged again following a study by Prostate Cancer UK (PCUK), which aims to establish if various testing strategies could tip the balance in the favour of a screening programme by detecting disease that the PSA test alone can miss.
Why is testing so important?
The goal of testing is to find and treat a cancer early. Testing can also help to monitor men who have already been diagnosed with prostate cancer, to ensure that the cancer does not recur or progress.
Despite the ongoing debate within the oncology community around the PSA test – there is general consensus surrounding the role of testing in early detection and improved survival rates.
Unfortunately, here in the UK, research has shown national testing rates lag behind best-practice recommendations for both biomarker testing for somatic (non-hereditary) mutations and other biomarkers, and for genetic testing.
Prostate cancer – why timing AND knowledge is everything
When found early, prostate cancer can be successfully treated.5 With greater awareness of the risk factors, signs, and symptoms to look out for, along with newer imaging techniques, we can make earlier diagnosis a reality for more men and their families in the UK.
Visit Prostate Cancer UK today to check your risk in 30 seconds.
References: prostatecanceruk.org, cancerresearchuk.org, ons.gov.uk, crukcancerintelligence, cancer.org
Lee Welch is Diagnostics Lead at AstraZeneca UK
AstraZeneca provided input into the development of the article, but not funding. Pharma Times had final editorial control.